Are reimbursement delays, rising administrative costs, and constant back-and-forth with payers quietly slowing your organization down? As volumes grow and margins tighten, many companies are turning to AI for claims processing to replace manual checks and fragmented workflows that still dominate back-office operations. That shift has moved the topic from an experimental idea to a practical conversation in executive meetings.
In this article, we explore how a more intelligent approach can reduce friction, improve predictability, and give decision makers clearer control over revenue cycles without adding complexity to everyday operations.
If you look closely at how reimbursement is still done in many organizations, the problem is rarely a lack of effort. Teams spend hours reviewing submissions, correcting small inconsistencies, and responding to payer requests, often under tight deadlines and with limited visibility into what happens next. Over time, this creates a cycle where experienced staff are tied up with repetitive tasks instead of focusing on exceptions and higher-value work.
In fact, a McKinsey report found that traditional manual claims workflows can take up to 23 days longer for complex cases compared to processes enhanced with intelligent automation, highlighting just how much time is lost in everyday operations.
Payments arrive later than expected, forecasting becomes less reliable, and administrative overhead quietly grows. Small errors turn into rework, rework turns into delays, and delays affect cash flow and planning. What makes this especially challenging is that many of these issues are not dramatic failures. They are everyday inefficiencies that accumulate and become part of normal operations:
As volumes increase and payer requirements continue to evolve, these traditional approaches struggle to keep up. Technically, the system still works, but at a cost that becomes harder to justify as the business scales.
When generative AI in claims processing starts supporting everyday tasks, the entire process becomes more deliberate and less chaotic. You no longer have to wait for feedback to understand what went wrong and identify risk points earlier, and allow submissions to be adjusted before they leave the system. Eventually, the operational pace becomes calmer, and avoidable corrections decrease.
Traditional procedures often revolve around response rather than prevention. Errors tend to surface only after a rejection or delay, which pushes teams into urgent rework. Artificial intelligence claims processing helps address inconsistencies upfront, reducing interruptions, stabilizing timelines, and making communication with payers more focused and less repetitive.
Maintaining uniform standards becomes challenging as reimbursement volumes grow. Teams may interpret the same rules in slightly different ways, leading to uneven outcomes. Centralized decision frameworks bring alignment to how submissions are prepared and reviewed. Over time, you see approval rates rise while uncertainty across departments decreases
Understanding where and why delays occur plays a critical role in long-term planning. Structured insight into performance replaces assumptions and fragmented feedback. Patterns related to specific payers, submission types, or internal handoffs become easier to recognize. Leadership gains a stronger footing when adjusting processes or planning growth.
Routine checks consume a large share of experienced staff time. Systematic handling of these tasks allows specialists to concentrate on complex cases that require judgment and context. Thus, the shift strengthens operational resilience and helps teams apply their knowledge where it has the greatest impact.
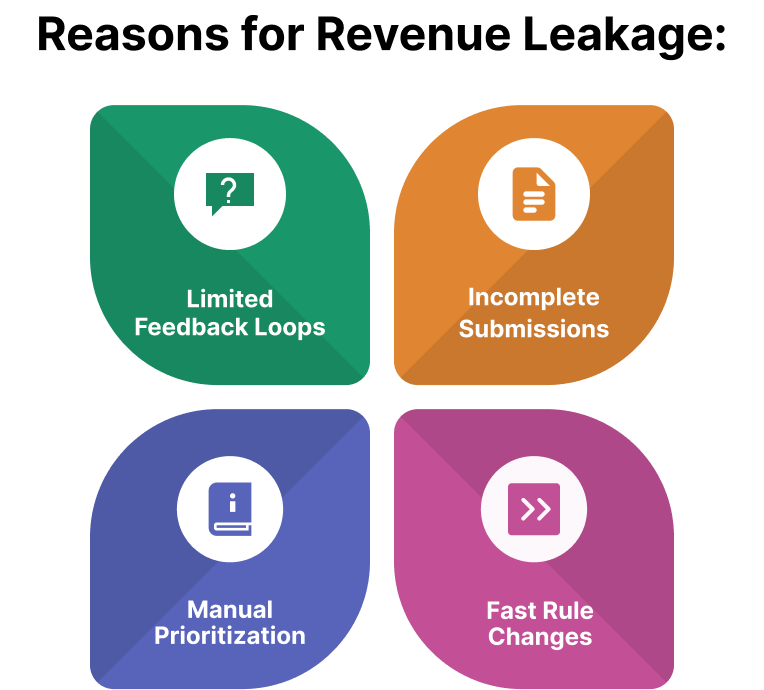
Revenue gaps rarely appear overnight. In most organizations, they develop gradually through small, repeated breakdowns in everyday work. A missing detail, an outdated rule, or a delayed response may seem insignificant on its own, yet together they create longer cycles and unpredictable outcomes. Over time, these issues start affecting cash flow and planning confidence.
Some organizations have already seen remarkable results by integrating AI healthcare software solutions into their procedures, offering a clear answer to how AI can be used in claims processing in real-world settings. These cases show how intelligent tools can streamline operations, speed up reimbursements, and free staff to focus on complex, high-value tasks.
A US-based healthcare provider partnered with CleverDev Software to build a custom AI claims processing solution tailored to their unique revenue cycle requirements. CleverDev developed an intelligent system that automatically classifies claim types, detects inconsistencies, and prioritizes high-risk or high-value claims for human review.
The solution integrated seamlessly with the provider’s existing workflow, enabling faster adjudication and reducing manual touchpoints without disrupting current operations. Over time, the provider experienced improved accuracy in claim submissions, faster reimbursement cycles, and a measurable reduction in denials and rework. With CleverDev’s custom approach, the organization was able to maintain compliance and oversight while scaling its claims operations efficiently.
Lemonade, a fully digital insurance company, has transformed the way they handle claims with its AI assistant, nicknamed “Jim.” The system can process simple claims almost instantly, sometimes settling cases in just a few seconds after customers upload photos or short videos. Their innovative approach dramatically reduces turnaround time, improves the customer experience, and allows human staff to focus on unusual or complex cases rather than routine verification.
Allstate is another remarkable case. They have introduced AI-based claims processing into workflows to assist with tasks like assessing vehicle damage from customer photos and generating consistent, clear communications. While adjusters still review cases, the tool speeds up routine processing, reduces manual workload, and ensures more accurate, predictable results. Such an organic combination of human expertise and intelligent support improves both efficiency and customer satisfaction.

Integrating smarter tools doesn’t mean overhauling every process overnight. When implemented thoughtfully, these approaches complement existing course and staff expertise, making operations smoother rather than more complicated.
In fact, research published in the European Journal of Computer Science and Information Technology found that organizations using AI in claims processing saw a 46% increase in throughput and significantly improved accuracy while maintaining compliance, showing measurable benefits from these modern workflows.
Let’s see how these technologies keep the focus on removing repetitive hurdles and giving teams the freedom to concentrate on higher-impact work.
Modern tools are designed to work alongside the platforms and processes already in place. Instead of replacing familiar interfaces, they connect to existing systems, providing guidance and oversight where it matters most. Staff can continue using the tools they know while benefiting from additional accuracy and efficiency.
Not every submission follows the same path. When irregularities arise, artificial intelligence in claims processing helps flag them quickly and directs them to the right specialist. Teams spend less time hunting for errors and more time resolving cases that truly need human attention.
The system generates performance insights automatically, providing a real-time view of where bottlenecks or errors occur. Management can see trends as they develop, which allows for proactive adjustments in staffing, process tweaks, or training.
With clearer visibility and consistent handling of submissions, different departments can work together more effectively. Shared rules and transparent reporting reduce misunderstandings and foster a sense of shared ownership over outcomes.
Operations remain flexible, but decisions become more informed, and everyday friction slowly diminishes. Staff can focus on judgment-heavy tasks, while routine hurdles are handled in the background, keeping workflows moving efficiently.
Adopting AI healthcare claims processing creates measurable effects touching some of the most important areas, such as expenses, timelines, and oversight.
Repetitive checks and corrections take a surprising portion of staff time. When staff handle those tasks systematically, they can focus on higher-value work instead of chasing avoidable errors. Fewer rework cycles and less overtime translate into noticeable savings and a healthier bottom line.
Every delay avoided with AI claims management software speeds up the overall reimbursement timeline. Submissions move through the system more smoothly, follow-ups happen sooner, and approvals arrive more predictably, improving cash flow and the ability to plan with confidence.
Leaders gain clearer insight into workflow performance, from individual submissions to team-level patterns. Trends in delays or errors become easier to spot, and resource allocation decisions can be made based on actual data rather than assumptions.
With improved consistency and fewer surprises, forecasting becomes more reliable. Financial planning, staffing, and strategic initiatives can be executed with confidence, knowing that operations are running on a foundation of repeatable and traceable processes.
The overall impact is a smoother, more manageable reimbursement cycle where resources are used effectively, timelines are shortened, and oversight is clearer, giving you peace of mind and stronger control over outcomes.

While the benefits are compelling, claims management software development also comes with practical challenges that are crucial to evaluate. Understanding these limitations early helps set realistic expectations and reduces the risk of disruption during adoption.
Many businesses rely on complex, long-established systems. Introducing agentic AI in claims processing into this environment requires careful integration planning. Without proper alignment, teams may face duplicated work, process friction, or inconsistent outcomes during the transition period.
Automated decision logic relies heavily on the quality and structure of incoming information. Inconsistent formats, missing fields, or outdated inputs can affect performance and require additional oversight and investment in standardization before seeing full value.
Adoption is not only a technical challenge but also a human one. Employees may initially hesitate to rely on automated recommendations, especially in high-stakes reimbursement work. Therefore, clear communication, training, and gradual rollout are essential to build confidence and ensure collaboration between staff and systems.
Agentic AI for claims processing is not a set-and-forget initiative. Payer rules, internal policies, and regulations continue to evolve. Regular monitoring, updates, and performance reviews are necessary to keep workflows accurate and aligned with business goals.
Healthcare reimbursement operates in a tightly regulated environment. Firms must ensure that automated decision logic remains transparent, auditable, and compliant with applicable standards. In turn, this requires governance structures that balance efficiency with accountability.
The good news is that when approached strategically, these challenges are manageable. Companies that plan carefully, involve stakeholders early, and prioritize transparency are far better positioned to realize long-term value while avoiding common pitfalls.
Introducing claim processing using AI requires careful planning. The goal is not simply to add technology but to ensure it fits seamlessly into operations, supports staff, and delivers measurable benefits. Attention to preparation and alignment can make the difference between a smooth transition and a frustrating disruption.
Overall, companies that take a thoughtful approach to AI-powered claims processing move toward greater stability and confidence in their operations. Fewer errors, clearer workflows, and better visibility reduce uncertainty and make day-to-day work easier to manage. As these improvements take hold, financial planning becomes more reliable, teams can spend more time on meaningful work, and leadership gains clearer insight into how the revenue cycle is performing. With deep expertise in building and integrating AI-driven solutions for complex workflows, CleverDev Software helps organizations design claims processing systems that deliver these gains while aligning seamlessly with existing operations.
When AI fits naturally into existing processes, its impact grows over time. Early issues are easier to spot, consistency improves across departments, and oversight remains clear without adding pressure. Therefore, you create a more controlled, more resilient revenue cycle that is better prepared for change.


Our newsletter is packed with valuable insights, exclusive offers, and helpful resources that can help you grow your business and achieve your goals.