What if the tools you rely on to run your organization weren’t just helpful but truly game-changing? That’s the very question behind the ongoing debate about the pros and cons of AI in healthcare, a topic that every decision-maker in the industry needs to understand before making their next big move.
The adoption of this technology introduced incremental change and shook the very foundations of how people are diagnosed, treated, and supported throughout their medical journeys. From the research labs driving discoveries to the frontlines of patient interaction, its influence is everywhere, leaving no corner untouched.
On the positive side, it’s opening doors to precision and personalization that were once unimaginable. Professionals now can spot early warning signs with greater accuracy, design tailored treatment paths, and reduce the guesswork that often slows down progress. At the same time, administrative teams are experiencing smoother workflows, which means less time wasted on repetitive tasks and more focus on what truly matters.
However, no revolution comes without its challenges. Concerns around implementation costs, trust in automated decision-making, and ethical considerations are sparking lively discussions across the industry. Leaders are weighing these opportunities against potential risks, carefully examining where the balance tips in their favor.
In this article, we’ll explore the pros and cons of using AI in healthcare, highlighting both the opportunities it creates and the challenges it raises, so you can see how it might impact your organization and guide smarter decisions.
The growing popularity of these innovations marks a turning point in the history of modern medicine. Over the past decade, they have shifted from experimental tools into essential drivers of progress, now viewed as a cornerstone of efficiency and innovation across medical practices worldwide. To understand when this rise truly began, it’s important to trace the milestones that brought it into the mainstream.
The early 2000s were the period when attention really started to build. Advances in computing power, the rise of large-scale datasets, and major improvements in algorithmic design created the right conditions for adoption. What had once been theoretical suddenly became practical, offering ways to solve long-standing challenges of integrated healthcare systems, such as improving diagnostic accuracy, designing more personalized treatments, and streamlining operations. This realization acted as the catalyst for broader interest and investment.
The scale of growth since then has been dramatic. Statista reports that the market is forecasted to reach $244.22 billion by 2025. From 2025 to 2031, it is expected to grow at an impressive annual rate of 26.6%, potentially reaching a total value of $1.01 trillion by 2031. Such rapid expansion demonstrates just how quickly adoption is accelerating, influencing not only hospitals and clinics but also pharmaceutical firms, biotechnology companies, and the wider medical ecosystem. As this momentum continues, these technologies are set to further reshape workflows, accelerate drug development, and redefine the delivery of patient care around the world.
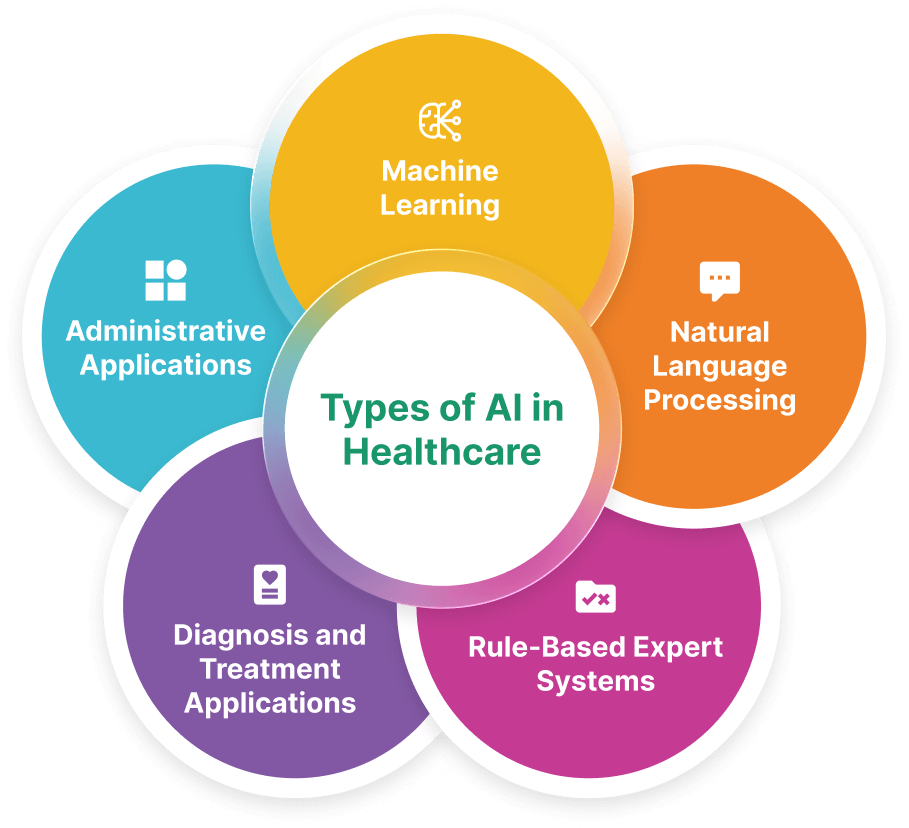
Understanding these different types is crucial for any business leader navigating a fast-changing industry. Each comes with strengths and limitations and knowing how they work guides smart investment and adoption decisions.
In the U.S., the healthcare sector is leading the way, with investments reaching $500 million in 2024, 67% higher than the next sector. This growth shows the potential of these innovations, but success depends on smooth integration, clear costs, and strong privacy protections.
Machine learning has quickly become a cornerstone in modern medicine. By identifying patterns across massive sets of clinical records, it helps professionals make more precise decisions, from spotting diseases earlier to tailoring treatment plans for individuals.
Think of it as having a second set of expert eyes that can scan thousands of medical images, track subtle changes in vital signs, and even predict how patients might respond to certain therapies. One of medical software development's most powerful uses is in precision medicine, where supervised learning helps determine the most effective treatment for each person.
A growing branch, deep learning, is pushing things even further, enabling tasks like speech recognition and more advanced image analysis in areas that are already changing how clinical teams work.
Another major area reshaping the industry is natural language processing. At its core, NLP allows off-the-shelf software to interpret and use human language. This means that piles of medical notes, test results, and historical records no longer need to remain locked in complex jargon and can be translated into actionable insights.
For instance, NLP can help identify the right treatment path by quickly pulling relevant details from records, predict risks by analyzing past histories, and even streamline communication between professionals. By cutting through complexity, NLP helps clinicians save valuable time while improving decision-making.
Expert systems laid the foundation long before today's algorithms. These rely on structured “if-then” rules crafted by specialists. While they’re easy to follow, their limitations become clear as the rulebooks expand into the thousands.
Updates are cumbersome, and rules can conflict with each other. Still, many systems in use today, especially clearinghouses in medical billing and electronic health records, continue to include this logic to support everyday decision-making.
Supporting doctors in diagnosing and treating patients has always been one of the most discussed uses of these technologies. Early versions struggled to outperform humans, but newer approaches are proving far more effective.
The main AI challenges in healthcare aren’t the accuracy of recommendations; it’s integrating them seamlessly into clinical workflows and record systems. Many current offerings remain standalone tools, addressing narrow tasks. For leaders, the key consideration here is whether to invest in costly integrations or partner with vendors that already build compatible systems.
Not all impact is clinical; administration is being transformed as well. From managing claims and entering records to scheduling appointments, repetitive tasks are now handled with far more speed and accuracy. Patient engagement software solutions not only reduce human error but also free professionals to spend more time on meaningful work. For organizations, this translates into both higher productivity and cost savings, while also improving the overall experience for patients.

When we look at how far the industry has come, two questions stand out: how has this wave of innovation truly changed the way care is delivered, and what are the benefits of AI in healthcare? The impact has been nothing short of remarkable, reshaping diagnostics, prevention, and even the way organizations manage their daily operations.
Advanced tools can now analyze scans like X-rays and MRIs faster and, in many cases, with the benefits of generative AI in healthcare, such as greater accuracy than the human eye alone.
Some of the most well-known conversational AI for healthcare have highlighted just how powerful this shift can be.
Another major advancement lies in predictive analytics, where patterns in patient histories are analyzed to forecast future risks.
It’s not only clinical care that’s being transformed — everyday operations are also becoming more efficient, creating a smoother experience for both organizations and the people they serve.
This transformation hasn’t happened overnight. Step by step, these advancements have become embedded in the medical field.

Innovative technology may hold enormous promise but bringing it into everyday practice isn’t as simple as flipping a switch. Business leaders and clinicians alike face hurdles that go beyond technical performance, ranging from patient trust to accountability, fairness, and the complexity of adoption.
Let’s unpack the pros and cons of AI in healthcare, focusing on the biggest roadblocks that stand in the way of progress.
Even when artificial intelligence in the healthcare business proves accurate, patients don’t automatically feel comfortable relying on it. Trust has to be earned through openness and reassurance.
Another major concern lies in the quality and diversity of training inputs. If the foundation isn’t balanced, results risk reflecting existing inequalities.
With greater autonomy comes greater questions about responsibility. One of the AI in healthcare cons is that if a recommendation causes harm, who is held accountable?
Even when new AI healthcare software solutions show impressive results in pilot projects, scaling them across an entire organization is another story.
Overall, with the right tools, you can quickly analyze vast amounts of information, identify potential issues before they become problems, and deliver personalized strategies that truly make a difference. Adopting these innovations allows you to streamline workflows, reduce operational costs, and improve efficiency across your organization. Ultimately, considering all the AI in healthcare pros and cons, this means better outcomes, smoother processes, and an enhanced experience for everyone you serve.
CleverDev Software designs technology tailored to drive real results, equipping you with tools that fit your business goals and fuel growth at every stage. Reach out to us today and discover how we can streamline your workflows, cut complexity, and help you achieve more with ease.


Our newsletter is packed with valuable insights, exclusive offers, and helpful resources that can help you grow your business and achieve your goals.